Are nursing home residents getting badly needed COVID boosters? Here’s why it’s hard to tell.
Cases of COVID-19 among Pennsylvania nursing home residents are up. “Fully vaccinated at this point should mean that you’ve been boosted, especially in this population,” one expert said.
In October and early November, 16 nursing home residents and one staff member at Philadelphia Protestant Home tested positive for COVID-19. Three people in independent living also got sick.
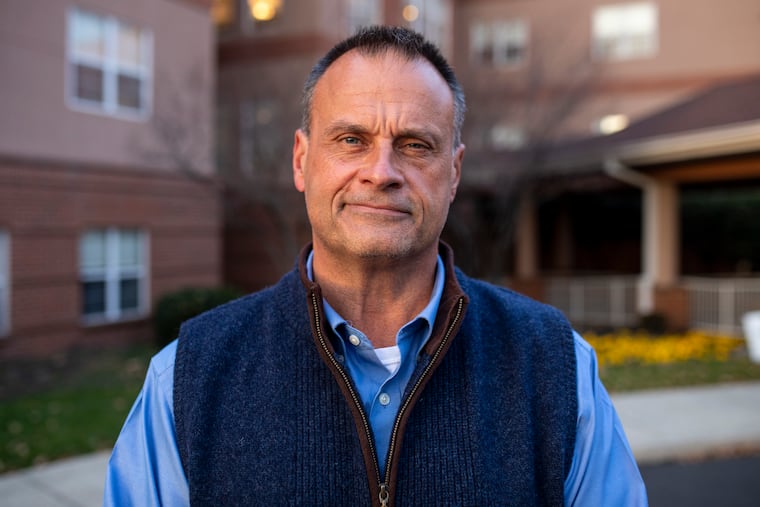
It was a strong sign that vaccine protection was waning in this vulnerable population eight months after almost all residents got their second shots. Every single case was a breakthrough infection, said John Dubyk, the Northeast Philadelphia retirement community’s president and CEO.
Two of the nursing home’s 57 residents died following infection.
The CDC had approved Pfizer boosters for people in nursing homes on Sept. 24. Dubyk said the first date he could schedule the shots was Nov. 2. They were received enthusiastically. There have been no new cases, he said, since Nov. 7.
Although the rise of the new variant, omicron, raises the specter of “more chaos” for his industry, Dubyk said boosters make him more confident that his facility can avoid another surge.
Gaps in federal and state reporting make it impossible to know whether other long-term care facilities have, like Philadelphia Protestant Home, been able to give boosters to most of their residents.
It is well-known, though, that nursing home residents are especially prone to serious illness and death from COVID-19. The virus burned through some facilities during its first assault on the United States last year. Nearly 138,000 residents have died. A combination of lockdowns, better access to protective equipment, and better treatment helped during subsequent waves, but cases really plummeted after vaccines became available earlier this year. However, because of their age and many health problems, nursing home residents have weaker immune systems, an added risk factor as vaccine protection weakened and the delta variant emerged. Nationally, about 1,400 residents have died in the last month, according to the CDC.
Meanwhile, the federal government recently removed restrictions on visiting nursing home residents, increasing the odds that infected family members could cause outbreaks among residents with weakened vaccine protection.
“This is a clarion call to get boosters into nursing homes for everyone,” said Susan Reinhard, senior vice president and executive director at AARP’s Public Policy Institute.
Nursing home leaders recognize how agonizing COVID lockdowns were for families and residents, but they’ve also seen how easily the virus infiltrates even strong defenses. “We’re fairly confident that it came from a visitor,” Dubyk said of his home’s recent outbreak.
Karl Steinberg, a San Diego geriatrician who is president of AMDA–the Society for Post‑Acute and Long‑Term Care, thinks the government should have prioritized getting nursing home residents boosters fast. “There’s no question that there’s waning immunity,” he said. Four fully vaccinated residents died at a facility near him recently. “It’s scary. We just don’t want another bloodbath of the kind we saw last winter.”
He thinks boosters are crucial for his patients. “Fully vaccinated at this point should mean that you’ve been boosted, especially in this population,” he said.
In Pennsylvania, Philadelphia Protestant Home is far from alone in having had a recent outbreak. A state report based on federal data last week showed that three other facilities in the Philadelphia region had more than 10 cases in the previous four weeks. The good news is that most had none or very few.
Statewide, three facilities reported 35 to 40 cases among residents in the previous four weeks and seven said they had more than 20. Seventeen more reported that more than 10 staff members had tested positive, including one facility with 40 infected employees. Officials at four homes with high numbers did not respond to calls.
Throughout the nation, residents were much quicker to embrace vaccines than staff members were. Private and government mandates have since reduced the gap between resident and employee vaccination rates.
Chiquita Brooks-LaSure, administrator of the Centers for Medicare & Medicaid Services, said the Biden administration has emphasized to long-term care facilities the importance of vaccination, including boosters, for all residents and staff. She said her agency plans to begin publicly reporting booster rates “in the next few weeks.”
Pennsylvania said it is waiting for CMS to report data. A New Jersey Health Department spokesperson said it would report booster information soon.
AARP’s Reinhard is frustrated by the lack of information. Because they were vaccinated so early, nursing home residents are obviously at risk, she said. “It seems to me it’s a no-brainer,” she said. “I have been saying this for months.” She urged family members to lobby for quick vaccination of their loved ones.
During a conference call last week, LeadingAge, an organization that represents nonprofit senior living providers, asked listeners about boosters. Of the 150 that responded, 91% said they had held booster clinics. Ninety-three percent said more than half of residents had accepted boosters.
Pattie Tucker, a spokesperson for the Health Care Association of New Jersey, said her executive director was told Thanksgiving week that 65% of residents and 29% of staff had received boosters.
Steinberg said that nursing home booster rates appear to be “hugely variable.” Some facilities in Los Angeles County have given boosters to 97% of residents, he said, while some in San Diego County, where he works, have done “much, much less.”
Daniel Haimowitz, a geriatrician who is medical director at nursing homes in Souderton and Langhorne, said booster uptake has been good, but some people are not thrilled to get a third jab. “To some degree, people don’t feel the same urgency that they used to feel,” he said.
Several government and senior care officials said they had heard of no barriers to providing boosters to nursing home residents and staff. Unlike earlier in the year, there’s plenty of supply and pharmacies have experience with the shots. However, a third of those polled by LeadingAge said they had faced “some challenges” in getting the shots.
Lynne Katzmann, founder and CEO of Juniper Communities, said she had heard of cases where clinics in nursing homes were canceled multiple times because pharmacy partners didn’t have enough staff to give the shots. “This is a labor issue,” she said. Juniper, which operates 30 communities in Pennsylvania, New Jersey, Texas, and Colorado, is now encouraging staff and residents who can travel to get their shots at neighborhood drugstores.
During a call with LeadingAge members on Dec. 1, Sonya Bernstein, senior adviser to the White House, said the CDC will now pair providers that are having trouble scheduling vaccine clinics with available pharmacies.
The good news is that medical directors and nursing home officials said vaccinated residents who have become infected have generally had mild symptoms. Several said they now offer monoclonal antibodies to residents who test positive. Some have also given the new drugs to uninfected residents who may have been exposed.
Kelli Mills, vice president of operations at Messiah Lifeways, a retirement community with about 800 residents in Mechanicsburg, said most infected residents who received monoclonal antibodies “rebounded well within 24 hours.” Two residents there — one in the nursing home and one in personal care — died during a small outbreak earlier this fall. The family of one of those patients decided against using monoclonal antibodies. There have been no new cases since 96% of residents got their boosters.
Haimowitz said he knows people are tired of hearing the same old refrain: Wash your hands. Keep your distance. Wear a mask. Get vaccinated. But those measures are especially important now, he said, as we enter the winter with a new variant in the wings. “We need not to let our guard down,” he said.
Mills knows that’s true. Messiah’s staff is ready with plenty of personal protective gear and months of pandemic experience. It’s the emotional component she’s worried about. “What in the world will we do if we have to go backwards?” she asked.