The FDA approves much-debated Alzheimer’s drug developed by Biogen
The new drug, which Biogen developed with Japan’s Eisai Co., did not reverse mental decline, only slowing it in one study.
WASHINGTON — Government health officials on Monday approved the first new drug for Alzheimer’s disease in nearly 20 years, disregarding warnings from independent advisers that the much-debated treatment hasn’t been shown to help slow the brain-destroying disease.
The Food and Drug Administration approved the drug from Biogen based on study results showing it seemed “reasonably likely” to benefit Alzheimer’s patients. It’s the only therapy that U.S. regulators have said can likely treat the underlying disease, rather than manage symptoms like anxiety and insomnia.
The decision, which could impact millions of Americans and their families, is certain to spark disagreements among physicians, medical researchers and patient groups. It also has far-reaching implications for the standards used to evaluate experimental therapies, including those that show only incremental benefits.
The new drug, which Biogen developed with Japan’s Eisai Co., did not reverse mental decline, only slowing it in one study. The medication, aducanumab, will be marketed as Aduhelm and is to be given as an infusion every four weeks.
» READ MORE: Penn dementia expert on newly approved Alzheimer’s drug: ‘The data aren’t strong enough’
Dr. Caleb Alexander, an FDA adviser who recommended against the drug’s approval, said he was “surprised and disappointed” by the decision.
“The FDA gets the respect that it does because it has regulatory standards that are based on firm evidence. In this case, I think they gave the product a pass,” said Alexander, a medical researcher at Johns Hopkins University.
The FDA’s top drug regulator acknowledged that “residual uncertainties” surround the drug, but said Aduhelm’s ability to reduce harmful clumps of plaque in the brain is expected to help slow dementia.
“The data supports patients and caregivers having the choice to use this drug,” Dr. Patrizia Cavazzoni told reporters. She said the FDA carefully weighed the input of people living with the “devastating, debilitating and deadly disease.”
Under terms of the so-called accelerated approval, the FDA is requiring Biogen to conduct a follow-up study to confirm benefits for patients. If the study fails to show effectiveness, the FDA could pull the drug from the market, though the agency rarely does so.
Biogen said the drug would cost approximately $56,000 for a typical year’s worth of treatment, and said the price would not be raised for four years. Most patients won’t pay anywhere near that thanks to insurance coverage and other discounts. The company said it aims to complete the FDA-mandated follow-up trial by 2030.
Biogen shares jumped 38% in trading Monday on the news, with analysts forecasting billions in future sales. The Cambridge, Massachusetts-based company plans to begin shipping millions of doses within two weeks.
The non-profit Institute for Clinical and Economic Review, which studies drug value, said Biogen’s drug would have to halt dementia entirely to justify its $56,000 per-year price tag.
Some 6 million people in the U.S. and many more worldwide have Alzheimer’s, which gradually attacks areas of the brain needed for memory, reasoning, communication and basic daily tasks. In the final stages of the disease, those afflicted lose the ability to swallow. The global burden of the disease, the most common cause of dementia, is only expected to grow as millions more baby boomers progress further into their 60s and 70s.
Aducanumab (pronounced “add-yoo-CAN-yoo-mab”) helps clear a protein called beta-amyloid from the brain. Other experimental drugs have done that but they made no difference in patients’ ability to think, care for themselves or live independently.
The pharmaceutical industry’s drug pipeline has been littered for years with failed Alzheimer’s treatments. The FDA’s greenlight Monday is likely to revive investments in therapies previously shelved by drugmakers.
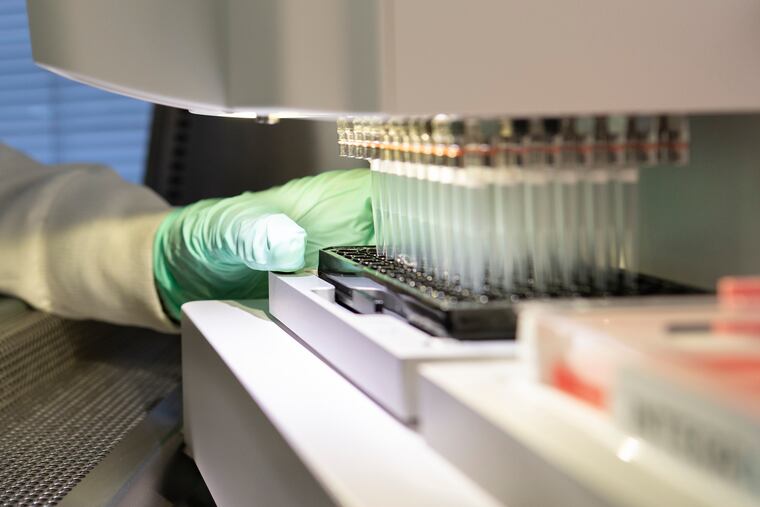
The new medicine is manufactured from living cells and will be given via infusion at a doctor’s office or hospital.
Researchers don’t fully understand what causes Alzheimer’s but there’s broad agreement the brain plaque targeted by aducanumab is just one contributor. Evidence suggests family history, education and chronic conditions like diabetes and heart disease may all play a role.
“This is a sign of hope but not the final answer,” said Dr. Richard Hodes, director of the National Institute on Aging, which wasn’t involved in the Biogen studies but funds research into how Alzheimer’s forms. “Amyloid is important but not the only contributing factor.”
Patients taking aducanumab saw their thinking skills decline 22% more slowly than patients taking a placebo.
But that meant a difference of just 0.39 on an 18-point score of cognitive and functional ability. And it’s unclear how such metrics translate into practical benefits, like greater independence or ability to recall important details.
The FDA’s review of the drug has become a flashpoint in longstanding debates over standards used to evaluate therapies for hard-to-treat conditions. On one side, groups representing Alzheimer’s patients and their families say any new therapy — even one of small benefit — warrants approval. But many experts warn that greenlighting the drug could set a dangerous precedent, opening the door to treatments of questionable benefit.
The approval came despite a scathing assessment in November by the FDA’s outside panel of neurological experts. The group voted “no” to a series of questions on whether reanalyzed data from a single study submitted by Biogen showed the drug was effective.
Biogen halted two studies in 2019 after disappointing results suggested aducanumab would not meet its goal of slowing mental and functional decline in Alzheimer’s patients.
Several months later, the company reversed course, announcing that a new analysis of one study showed the drug was effective at higher doses and the FDA had advised that it warranted review. Company scientists said the drug’s initial failure was due to some patients not receiving high enough doses to slow the disease.
But the changes to dosing and the company’s after-the-fact analysis made the results hard to interpret, raising skepticism among many experts, including those on the FDA panel.
The FDA isn’t required to follow the advice of its outside panelists and has previously disregarded their input when making similarly high-profile drug decisions.
About 900 U.S. medical facilities are ready to begin prescribing the drug, according to Biogen, with many more expected in coming months. But key practical questions remain: How long do patients benefit? How do physicians determine when to discontinue the drug? Does the drug have any benefit in patients with more advanced dementia?
With FDA approval, aducanumab is almost certain to be covered by most insurers, including Medicare, the government plan for seniors that covers more than 60 million people.
Insurers could try to manage the drug’s costs by requiring strict conditions, including brain scans to confirm plaque, before agreeing to cover it.
Additional scans will be needed to monitor potential side effects. The drug carries a warning about temporary brain swelling that can sometimes cause headaches, confusion and dizziness. Other side effects included allergic reactions, diarrhea and disorientation.
Although Biogen studied the drug in people with mild dementia or early-stage Alzheimer’s, the FDA label approved the drug for anyone with Alzheimer’s, a sweeping population given doctors have broad leeway in diagnosing the condition.
“The FDA is empowering the physician to make the decision on diagnosis,” Biogen CEO Michel Vounatsos said in an interview.
For patients already enrolled in Biogen’s trials, Monday’s announcement means they can continue taking a drug many believe has helped.
Phillip Lynn, 63, was diagnosed with Alzheimer’s in the spring of 2017 after having trouble with conversation and memory, including forgetting a recent vacation to Hawaii.
His husband Kurt Rehwinkel says Lynn’s cognitive ability has stabilized since starting on Biogen’s drug more than three years ago. And his performance on short-term memory tests has actually improved, though the couple acknowledges most patients are unlikely to see similar results.
“But even for those who it has little or no effect, I think hope is a good thing,” said Rehwinkel. “I don’t think there’s such a thing as false hope.”