Primary care is so much more than you may think | Expert Opinion
Patients call on their "family doctors" to see them through specialist visits and other diagnoses – and to counsel them when required.
The other day, one of my long-standing patients — a retired contractor in his mid-70s — scheduled an urgent appointment to see me in the office. He left no details about his symptoms, and I recall feeling curious walking into the exam room, uncertain what sort of medical issue I would encounter.
I found him sitting on the exam table looking worried, but in no physical distress. He was not feeling sick, but came in to seek my opinion on his pulmonologist’s proposed treatment plan for a recently discovered lung nodule that could be cancer.
He said the specialist recommended a CT scan for a more detailed view of the nodule, and then a biopsy if there were features suspicious for cancer. It sounded fairly straightforward, so I asked him to explain his concerns. He worried this would lead down a debilitating pathway that might keep him from caring for his wife (also my patient) who suffers from advanced dementia.
As we discussed various options to manage this complex and very personal dilemma, I felt gratified that he reached out to me, his primary care doctor, for guidance. I am not specialized in the nuanced management of lung nodules, but I know the context of his life, as well as how medicine works. I understand how his decisions may not fit neatly into the standard evaluation and treatment protocol.
This is primary care.
Another patient, a woman in her 50s who was less familiar to me, had come in earlier in the week with a cough that would not let up. She developed cold symptoms after returning from a vacation cruise; the aches and fatigue resolved after a few days, but her cough had now lingered for two weeks.
She was worried her infection had returned. After a thorough exam, I reassured her that she did not appear to have an infection and explained that sometimes coughing can persist for some time after a respiratory virus.
I did not offer a specific diagnosis, but we came up with a plan to control her symptoms and — most importantly — stay in close contact until it resolved completely. As I watched her tense shoulders slowly drop and her face soften, I was awed by how diagnosing someone’s concern can be just as meaningful and satisfying as diagnosing a disease.
This too, is primary care.
Commonly acknowledged as healthcare’s foundation, primary care is often the first touchpoint for diagnosis and treatment of acute and chronic conditions, preventive care, and a referral to specialists.
These are certainly core skills, but you may not realize how often patients seek counsel from their primary care providers to navigate highly specialized assessments and challenging treatment decisions, or for concerns without a clear diagnosis. (Unless, of course, you are one of the many who has actually done so.)
» READ MORE: A primary care clinician can help you through the healthcare 'rabbit hole.'.'.
In my 30 years of primary care practice, I have been amazed at how clinical problems can be common and repetitive, but people’s lives, perspectives, and circumstances are always unique and interesting.
The term primary care suggests a lack of specialization, but our expertise is the patient-doctor relationship and problem solving by carefully listening to the stories of patients we have come to know.
For me and many colleagues, this is among the most rewarding parts of medical practice. It also ranks high on the priority scale for what patients want in a physician — namely, the willingness to listen and respond to concerns. This is not the part of our work that causes physician burnout either; in fact, it may actually be part of the solution.
When concerns are raised about supporting and sustaining primary care, it is especially these nuanced conversations, matters that require trusting relationships and problems that do not fit neatly into a category of medical care.
These assessments can be initiated at an urgent care, emergency room, virtual clinic — or perhaps even by a chatbot — but connection and continuity are needed to resolve them. Much of what we do in primary care may be assisted — or even someday replaced — by new technology. But meaningful challenges will always require a unique human touch.
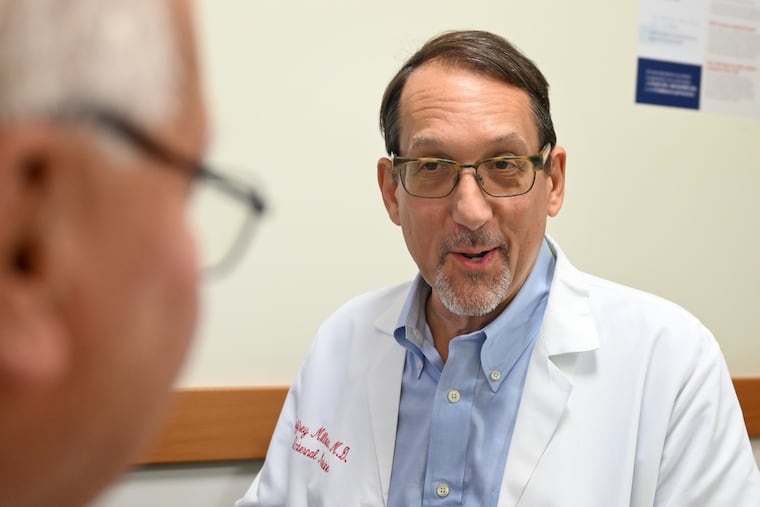
Jeffrey Millstein is an internist and regional medical director for Penn Primary Care.