When their body is the battleground, what does fighting disease really mean to patients?
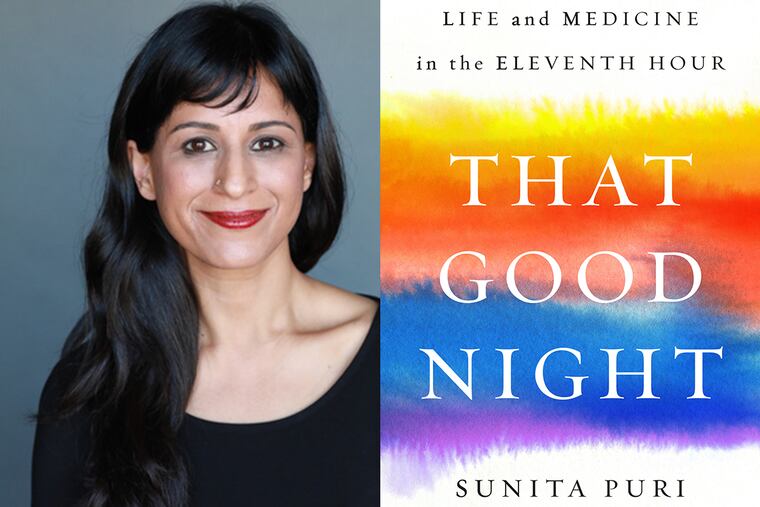
In this excerpt from her book "That Good Night," palliative care physician Sunita Puri explores what it means to regard illness like a war to be won at any cost.
Around the time I met Joe Brown, I realized that I doubled as an accidental linguist, helping patients and families to excavate the many layers of meaning they assign to a word or phrase. In the first few minutes of our conversation, Teresa [Joe’s daughter] would describe Joe as a “fighter.”
Countless patients described themselves this way to me. When I first met her, Linda had described herself as a “warrior” against her failing kidneys. Back in fellowship, Dave told me he felt more like a “soldier” in his “battle against emphysema” than he ever felt he’d been in Vietnam. Recently, I’d seen an elderly patient with end-stage lung cancer hospitalized with severe pneumonia. Her granddaughters superimposed an image of her face — thinned by cancer, crusted over with a slowly healing zoster rash — onto Hulk Hogan’s body, and hung photocopies on every wall in her room.
“Don’t be fooled by her looks. My grandma is every bit as tough as the Hulk and there’s no way she’s losing to this wimpy old cancer!” her granddaughter said when I first met her. Her grandmother moaned, trying again to remove the oxygen mask over her nose and mouth. “See? She’s so strong, she thinks she can fight this without even the oxygen!”
I understood this impulse to fight. When faced with anything life threatening, our instinct to preserve our lives is so strong that it’s practically a biological response to fight an enemy in every way possible. Our bodies want to keep living, which is why they have so many built-in mechanisms to stay alive even when faced with life-threatening illnesses or injuries. When, for example, heart failure worsens, the kidneys work harder to preserve blood pressure. If we suffer blood loss in a car accident, the heart pumps harder and faster, and our rate of breathing increases to meet the body’s needs for blood and oxygen. But what do we fight for when, despite the best possible effort made by the body and mind and medicine, the disease grows stronger?
In residency and the early months of fellowship, I had the impression that self-described fighters would be difficult patients. Fighters were the ones who didn’t actually understand how sick they were. They demanded unrealistic treatments and berated doctors who wouldn’t provide them.
They vocalized their courage and strength more loudly as their bodies weakened, as though the militaristic ferocity of their words alone could halt or reverse the territorial gains of their invisible enemy, be it cancer or heart disease or liver failure. When fighters died, their obituaries underscored their battles. Celebrities who died of cancer “lost their long battles” or “succumbed despite fighting.”
But what did these fighting words actually mean to the people who used them? Their use had become so pervasive that they were now de rigueur descriptors for anyone confronting mortality. Fighters wanted “everything” done to treat their disease. Fighters hoped for “miracles.” They refused to entertain any discussion of “giving up.”
Some physicians I knew interpreted the descriptor “fighter” as an indication that they should provide all treatments possible, regardless of their harm. Who were they, as physicians, to challenge or unpack the word “miracle”?
I had seen many a conversation stalled with the use of these phrases, and began to wonder if the way to advance a challenging discussion was to explore these word choices, to force clarity about what fighting for a miracle might mean in a very specific set of unfortunate circumstances. After all, didn’t the word “fight” imply a conflict? Did the fighter grasp the complexity and nuance of the battle? What did the fighter know about his or her enemy? How, specifically, did they understand the consequences of the fight, and what they were fighting for? How did they define “giving up”? What was worth fighting for? With what consequences for the battleground, which was inevitably one’s body and life? Could there be miracles aside from curing a disease, especially if that wasn’t possible?
The body has its own language, and Western medicine has become its adept interpreter. Using a blood pressure cuff, we can identify high blood pressure as the cause of chest pain. Through blood and urine samples, we can tell whether a person’s confusion is due to failing organs or an infection or taking too much of a certain medicine.
But do we know how to listen when the body tries to tell us that it is dying despite our best efforts to forestall death? If we are giving patients the weapons to fight these so-called battles, isn’t it our responsibility to help them understand what may and may not be possible to fight for, with what ammunition, and with what consequences? Doesn’t that merit as much discussion as the ways in which a patient may want to fight?
As I thought about Mr. Brown’s predicament, I felt myself reaching for the language my father gave me years before about the body: that it was our home but not our identity, that it was scientifically known but infinitely mysterious, that we could try to make it bend to our will but nature would always prevail. I’d fought to understand this duality when my own life and well-being hung in the balance, but it had taken years for me to move from intellectually understanding this concept to inhabiting it with more ease.
The soul wears the body like a cloth and discards it at the time of death. I wondered if I could use these words to help Mr. Brown.
Reprinted from That Good Night, by Sunita Puri, published by Viking, an imprint of Penguin Publishing Group, a division of Penguin Random House, LLC. Copyright © 2019 by Sunita Puri. Puri will be the keynote speaker at The Inquirer’s “Telling Your Health Story” event on Sept. 28. For tickets: inquirer.com/healthstory.