Q&A: Am I at risk for peripheral artery disease?
In a person with peripheral artery disease, the oxygenated blood is not able to adequately get to the limb due to an abnormality of the arteries, usually narrowing from plaque or sometimes being completely blocked.
Q: What is peripheral artery disease? Who is at risk?
A: Your arteries carry oxygenated blood away from your heart to your brain, arms, legs, and organs in the circulatory system. Your veins return the deoxygenated blood to your heart. In a person with peripheral artery disease (PAD), the oxygenated blood is not able to adequately get to the limb due to an abnormality of the arteries, usually narrowing from plaque or sometimes being completely blocked. Symptoms can develop, including pain with exercise, pain when sleeping at night, toe wounds, or even gangrene.
People at risk for developing PAD are those age 50 or older, those who have family history of PAD, or those who smoke. Other risk factors include artery disease in other regions of the body, such as heart disease with a history of heart attack; or carotid disease including a history of stroke. Diabetes and high cholesterol levels are also risk factors for the disease.
If you may be at risk, talk with your health-care provider about a non-invasive screening for PAD. The Ankle Brachial Index (ABI) and Pulse volume recordings (PVRs) include a comparison of the blood pressures and wave forms at different levels of the legs and the arms. Ultrasound with color-flow imaging (duplex) helps us evaluate the blood vessels and any degree of narrowing. In select cases, we use computed tomography angiography, magnetic resonance angiography, or fluoroscopic angiography to view the arteries.
We can treat PAD in a variety of ways. Medications can help decrease the progression of the disease. Antiplatelet therapy and cholesterol-lowering medication known as statin therapy may be recommended for patients with risk factors or known PAD. Additional medications might help to expand the blood vessels. Quitting smoking is very important for decreasing the risk of developing PAD, as well as lessening the progression of disease.
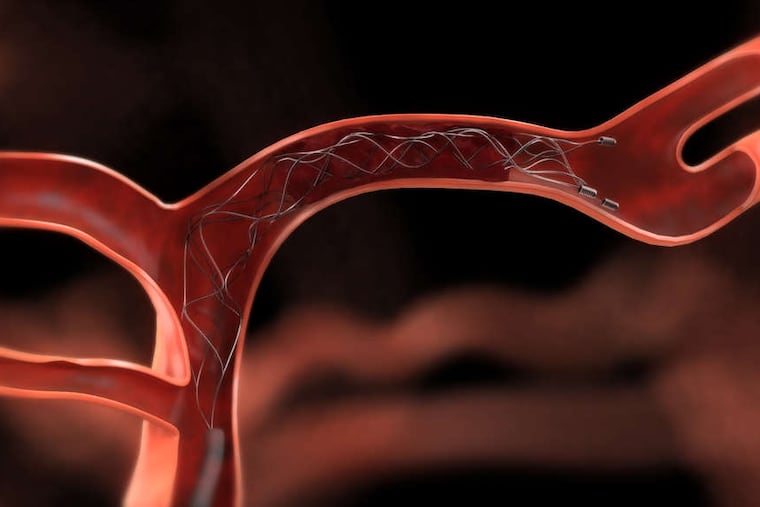
We might recommend exercise therapy and/or surgery based on the extent of disease and symptoms. If a procedure is required, we can perform minimally invasive surgery without big incisions in most cases. This is known as an endovascular – or inside the blood vessel – approach. It can involve angioplasty, through which we use a temporary balloon to widen a narrowed area in the artery. We might place a stent into the artery to help keep the diseased artery open. Another procedure to remove plaque endovascularly is an atherectomy. Sometimes open surgery is required, as well, and this may include removal of plaque or bypassing from one healthy blood vessel to another.
Severe untreated cases of PAD can lead to amputation of a finger, toe, arm, or leg. Gangrene can also lead to severe life-threatening infection. If we catch PAD early enough, we can save arms and legs and enhance quality of life with revascularization.
I recently cared for someone who had patches of gangrene on her foot and significant pain that limited her ability to walk. Given the extent of arterial blockage, she could have been facing amputation, but I performed a complex minimally invasive endovascular revascularization procedure with local anesthetic and minimal sedation. Her wounds have healed completely and she is walking without difficulty.
Chenée Tyson is a vascular surgeon at AtlantiCare Regional Medical Center in Pomona, N.J.