Q&A: Could a fractured bone from a fall be a sign of a more serious issue?
Postmenopausal osteoporosis occurs when the normal process of bone breakdown and bone formation changes due to a lack of estrogen.
Q: Could a fractured bone from a fall be a sign of a more serious issue?
A: I recently saw a 62-year-old female patient who was clearing the snow off her car in the unexpected November storm when she fell and broke her wrist. Her astute primary care provider told her that her broken bone was an early sign of bone loss and she needed a bone density scan.
Her scan, also known as a DEXA scan, showed severe osteoporosis. Her chance of having another fracture in the next year was 20 percent, and in the next five years over 50 percent. She was like many postmenopausal women who don’t realize that osteoporosis often leads to a broken bone after what may seem like a minor accident.
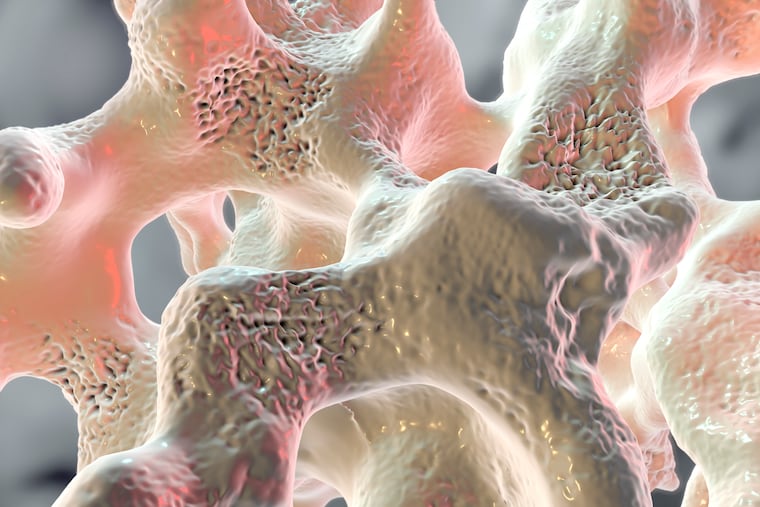
Postmenopausal osteoporosis occurs when the normal process of bone breakdown and bone formation changes due to a lack of estrogen. While many risk factors for bone loss exist, menopause is the most common. Women hit their peak bone mass in their mid-20s and slowly lose bone density until menopause, when the loss becomes much more dramatic.
Nearly 50 percent of American women over age 50 will suffer a fragility fracture in their lifetime. Fragility fractures — low-impact and low-velocity fractures that occur from a standing height or less — are the result of common falls. Missing the bottom step on the stairs, falling in the bathtub, or slipping on ice outside are all examples of falls that cause fragility fractures.
There are two types of treatment options available for postmenopausal osteoporosis: medications that prevent further bone loss and medications that build bone.
To build bone, one specific option is Tymlos (abaloparatide), approved by the U.S. Food and Drug Administration in 2017. This is a daily injection that stimulates the body’s natural bone-building cells, but should be limited to two years of use in a lifetime.
Examples of medication that prevents further bone loss are Fosamax (alendronate), Boniva (ibandronate), and Prolia (denosumab) which are available in various formulations.
Women with postmenopausal osteoporosis should talk with their healthcare professionals about what treatment options may be best for them, and do the following to avoid fractures:
consume 1200 mg of calcium via diet (and supplements, if necessary)
take a daily vitamin D supplement
engage in weight-bearing exercise 150 minutes a week
stop smoking
limit alcohol intake to seven drinks per week
To learn more about this disease, visit BoneNews.com and NOF.org where there are great resources for patients and healthcare providers alike.
Jacqi Kernaghan, PA-C, is a certified physician assistant at Crozer-Keystone Health System.