Panel recommends giving hepatitis C drugs to more Pa. Medicaid patients
MECHANICSBURG, Pa. - A state advisory committee, wading into one of the most fraught issues facing health-care policymakers, recommended Tuesday that Pennsylvania's Medicaid program pay to treat all patients infected with hepatitis C.
MECHANICSBURG, Pa. - A state advisory committee, wading into one of the most fraught issues facing health-care policymakers, recommended Tuesday that Pennsylvania's Medicaid program pay to treat all patients infected with hepatitis C.
The recommendation led to cheers - instead of the planned chants - from a dozen advocates who had been standing by quietly, not expecting the vote to go their way.
The first new treatments that can effectively cure more than 90 percent of hepatitis C infections began coming on the market two years ago. They cost up to $80,000 for a course of treatment, although Medicaid programs get discounts that can cut that amount in half.
As a result, many states have imposed strict approval guidelines even as Medicare and commercial insurers have been covering most treatments. More than three million Americans are estimated to be infected with hepatitis C. Symptoms may not appear for decades. But the eventual liver damage can be severe, leading to cirrhosis and cancer that can end up costing far more than treating the infection itself.
New Jersey has among the tightest guidelines in the country in its Medicaid program. Pennsylvania last year eased its requirements somewhat but still rejects large numbers of requests from doctors whose patients have the disease but have not yet developed liver damage.
Meeting in Mechanicsburg on Tuesday, the Pharmacy and Therapeutics Committee voted 10-7, with two abstentions, to lift the restrictions. The recommendation now goes to Ted Dallas, secretary of human services. It applies only to patients in the fee-for-service part of Medicaid, a tiny sliver of the total. but state policy requires that managed care organizations, which cover the vast majority, offer substantially similar coverage.
The secretary typically follows committee recommendations, but the numbers of potential hepatitis C patients and the cost of the drugs make this a special case.
Terri Cathers, the committee chair and pharmacy director for Medicaid, said after the meeting that while cost was a consideration for the committee, it could play a bigger role in the final decision.
"As a clinician, everyone who has this diagnosis should be treated," Cathers said, pointing to guidelines from infectious disease and liver organizations. "We should prevent people from getting so sick that they die."
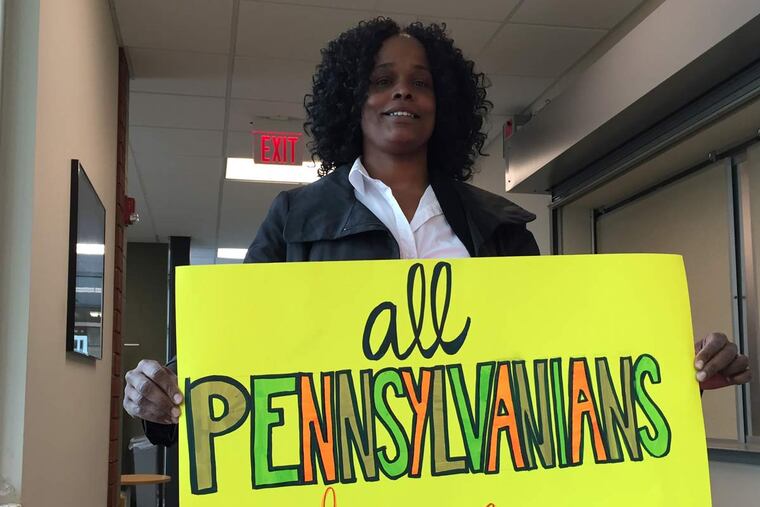
Tawanda Preston, who had been holding up a sign saying "All Pennsylvanians Deserve Access," left the room energized after the vote.
A patient navigator for an infectious disease clinic at Drexel University, Preston said some people who had tested positive in a mobile lab two years ago still had not been approved despite requests filed every six months. "I'm excited because this allows people who really need treatment to get cured," she said.
215-854-2617 @DonSapatkin