Post-Roe, contraceptive failures carry bigger stakes
The failure rate for typical use of birth control pills is 7%. For every million women taking pills, 70,000 unplanned pregnancies could occur in a year.
“No one walks into my office and says, ‘I plan on missing a pill,’” said obstetrician-gynecologist Mitchell Creinin.
“There is no such thing as perfect use; we are all real-life users,” said Creinin, a professor at the University of California-Davis who wrote a widely used textbook that details contraceptive failure rates.
Even when the odds of contraception failure are small, the number of incidents can add up quickly. More than 47 million women of reproductive age in the United States use contraception and, depending on the birth control method, hundreds of thousands of unplanned pregnancies can occur each year. With most abortions outlawed in at least 13 states and legal battles underway in others, contraceptive failures now carry bigger stakes for tens of millions of Americans.
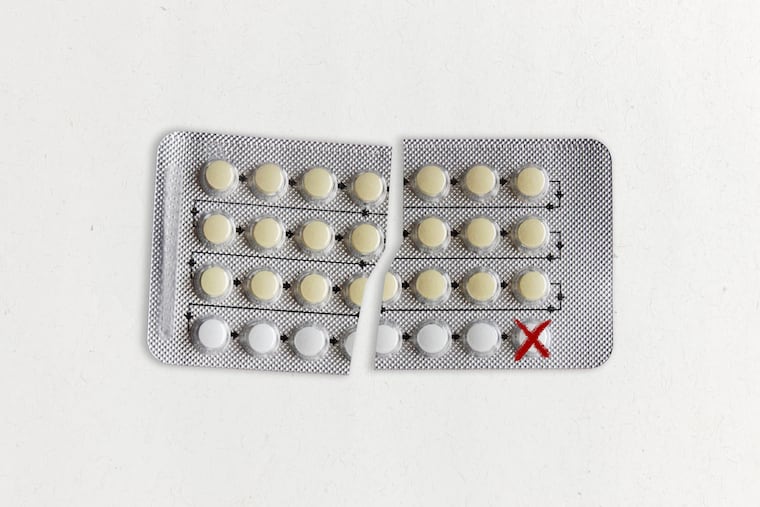
Researchers distinguish between the perfect use of birth control, when a method is used consistently and correctly every time, and typical use, when a method is used in real-life circumstances. No birth control, short of a complete female sterilization, has a 0.00% failure rate.
The failure rate for typical use of birth control pills is 7%. For every million women taking pills, 70,000 unplanned pregnancies could occur in a year. According to the most recent data available, more than 6.5 million women ages 15 to 49 use oral contraceptives, leading to about 460,000 unplanned pregnancies.
Even seemingly minuscule failure rates of IUDs and birth control implants can lead to surprises.
An intrauterine device releases a hormone that thickens the mucus on the cervix. Sperm hit the brick wall of mucus and are unable to pass through the barrier. Implants are matchstick-sized plastic rods placed under the skin, which send a steady, low dose of hormone into the body that also thickens the cervical mucus and prevents the ovaries from releasing an egg. But not always. The hormonal IUD and implants fail to prevent pregnancy 0.1% to 0.4% of the time.
About 4.8 million women use IUDs or implants in the U.S., leading to as many as 5,000 to 20,000 unplanned pregnancies a year.
“We’ve had women come through here for abortions who had an IUD, and they were the one in a thousand,” said Gordon Low, a nurse practitioner at the Planned Parenthood in Little Rock.
Abortion has been outlawed in Arkansas since the Supreme Court’s ruling on Dobbs v. Jackson Women’s Health Organization in late June. The only exception is when a patient’s death is considered imminent.
Those stakes are the new backdrop for people making decisions about which form of contraception to choose or calculating the chances of pregnancy.
Another complication is the belief among many that contraceptives should work all the time, every time.
“In medicine, there is never anything that is 100%,” said Régine Sitruk-Ware, a reproductive endocrinologist at the Population Council, a nonprofit research organization.
All sorts of factors interfere with contraceptive efficacy, said Sitruk-Ware. Certain medications for HIV and tuberculosis and the herbal supplement St. John’s wort can disrupt the liver’s processing of birth control pills. A medical provider might insert an IUD imprecisely into the uterus. Emergency contraception, including Plan B, is less effective in women weighing more than 165 pounds because the hormone in the medication is weight-dependent.
And life is hectic.
“You may have a delay in taking your next pill,” said Sitruk-Ware, or getting to the doctor to insert your next vaginal ring.
» READ MORE: Four Philly abortion providers talk about the calling that drives them to do emotionally challenging work
Using contraception consistently and correctly lessens the chance for a failure but Alina Salganicoff, KFF’s director of women’s health policy, said that for many people access to birth control is anything but dependable. Birth control pills are needed month after month, year after year, but “the vast majority of women can only get a one- to two-month supply,” she said.
Even vasectomies can fail.
During a vasectomy, the surgeon cuts the tube that carries sperm to the semen.
The procedure is one of the most effective methods of birth control — the failure rate is 0.15% — and avoids the side effects of hormonal birth control. But even after the vas deferens is cut, cells in the body can heal themselves, including after a vasectomy.
“If you get a cut on your finger, the skin covers it back up,” said Creinin. “Depending on how big the gap is and how the procedure is done, that tube may grow back together, and that’s one of the ways in which it fails.”
Researchers are testing reversible birth control methods for men, including a hormonal gel applied to the shoulders that suppresses sperm production. Among the 350 participants in the trial and their partners, so far zero pregnancies have occurred. It’s expected to take years for the new methods to reach the market and be available to consumers. Meanwhile, vasectomies and condoms remain the only contraception available for men, who remain fertile for much of their lives.
At 13%, the typical-use failure rate of condoms is among the highest of birth control methods. Condoms play a vital role in stopping the spread of HIV and other sexually transmitted infections, but they are often misused or tear. The typical-use failure rate means that for 1 million couples using condoms, 130,000 unplanned pregnancies could occur in one year.
Navigating the failure rates of birth control medicines and medical devices is just one aspect of preventing pregnancy. Ensuring a male sexual partner uses a condom can require negotiation or persuasion skills that can be difficult to navigate, said Jennifer Evans, an assistant teaching professor and health education specialist at Northeastern University.
Historically, women have had little to no say in whether to engage in sexual intercourse and limited autonomy over their bodies, complicating sexual-negotiation skills today, said Evans.
Part of Evans’ research focuses on men who coerce women into sex without a condom. One tactic known as “stealthing” is when a man puts on a condom but then removes it either before or during sexual intercourse without the other person’s knowledge or consent.
“In a lot of these stealthing cases women don’t necessarily know the condom has been used improperly,” Evans said. “It means they can’t engage in any kind of preventative behaviors like taking a Plan B or even going and getting an abortion in a timely manner.”
Evans has found that heterosexual men who engage in stealthing often have hostile attitudes toward women. They report that sex without a condom feels better or say they do it “for the thrill of engaging in a behavior they know is not OK,” she said. Evans cautions women who suspect a sexual partner will not use a condom correctly to not have sex with that person.
“The consequences were already severe before,” Evans said, “but now that Roe v. Wade has been overturned, they’re even more right now.”
This story is a collaboration between Kaiser Health News and Science Friday. Kaiser Health News is a national newsroom that covers health issues.