Uncontrolled diabetes can lead to serious eye problems
Three years ago, Allison Turner noticed her vision was getting a little blurry. "I knew I had to see a doctor," she said. "But I was scared and didn't deal with it."
Three years ago, Allison Turner noticed her vision was getting a little blurry.
"I knew I had to see a doctor," she said. "But I was scared and didn't deal with it."
The result was that when Turner, a professor of public policy and administration at West Chester University, awoke one morning, she couldn't see out of her left eye. A trip to a retina specialist confirmed she had suffered a detached retina caused by diabetic retinopathy.
Despite having had type 1 diabetes since she was 12, Turner, 36, never anticipated such a serious complication so early. In type 1, the body fails to make insulin, compared with type 2, in which the body cannot use the insulin it makes. But eye problems can be a complication for both types.
"I knew eye complications were a possibility," she said, "but they were abstract to me. I never thought it was something I'd have to worry about in my 30s."
Now, after four surgeries to reattach her retina and remove scar tissue inside her eye, Turner is legally blind in her left eye.
Despite medical advances, diabetes remains the top cause of blindness among working-age Americans between ages 20 and 60. About 10 percent of Americans have diabetes and those numbers are growing. Regionally, the number is as high as 20 percent, or one out of five people, according to Allen Ho, director of retina research at Wills Eye Hospital.
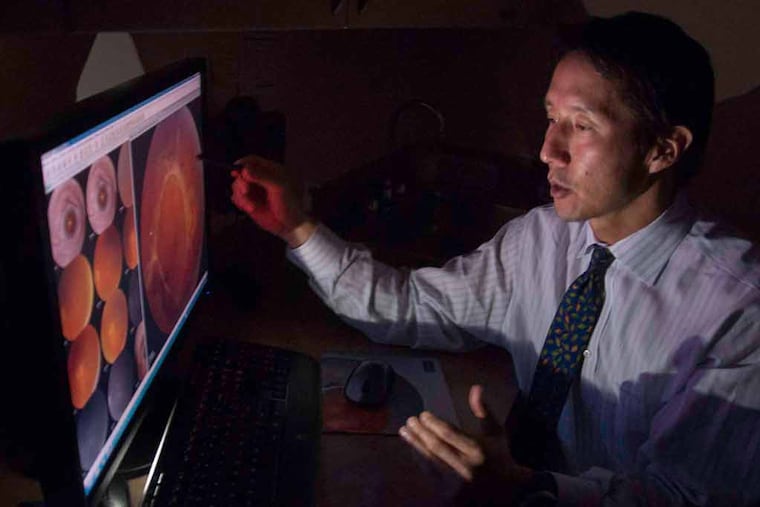
High blood-sugar levels caused by diabetes are toxic to the linings of blood vessels throughout the body, said Jason Hsu, a retina specialist at Wills Eye.
"Over time, the vessel walls get damaged, and the vessels develop microaneurysms, which can burst open and spread little spots of blood over the retina," he said. "Damaged vessels can also leak water, which causes swelling in the retina."
As the disease progresses, it can spur abnormal blood-vessel growth and swelling into the macula, the part of the eye responsible for straight-ahead, sharp vision. That can lead to blurred vision and, if left untreated, blindness.
Diabetic retinopathy can also cause a condition called diabetic macular edema.
"The retina is supposed to be watertight, but in a diabetic patient, in the face of fluctuating sugars, plasma leaks out and causes surrounding tissues to swell," said Josh Greene, a retina specialist in Northeast Philadelphia. "This fluid can leak into the center of the macula, the part of the eye where sharp straight-ahead vision occurs."
Macular edema can cause blurred vision or, if left untreated, blindness.
"The most important thing is not to be afraid of care, but to be more afraid of complications," said Ho. "We can prevent blindness in 90 percent of patients or greater if patients can get over barriers of fear or denial."
Which means that even if you have no trouble reading the mail or watching TV, if you have diabetes, you need to have a yearly eye exam.
"Someone who can do a front-to-back-of-the-eye exam is very important," said Ho.
"It's often a silent disease," said Hsu. "A lot of people don't realize they have the disease, because even with an advanced case, they might come in because they notice a few little floaters - which are caused by blood in the jelly of the eye. They may only notice a small change, but when we look in the eye, we realize that their vision is about to crash because all of these abnormal blood vessels are starting to bleed, pull at the retina, and cause a detachment. "
Loss of vision can occur suddenly, or it can be slow and progressive. And though diabetic retinopathy can improve, the general consensus is that it cannot be totally reversed.
That said, "lots of good studies show that controlling blood sugars and blood pressure lower the rate of retinopathy worsening," said Hsu. "It's very important to control sugar levels to prevent further damage."
To take care of retinopathy, patients are urged to make sure they have a primary doctor or endocrinologist to help with blood-sugar management, to keep to a low carbohydrate diet, and to control their blood pressure and levels of cholesterol.
Turner acknowledges her diabetes care had slipped in the months before her retina detached.
"I think I was still young enough to feel that I could not tend to it very well and not feel really bad," she says. "The younger you are, the more you feel you can power through high and low blood sugars without too many physical consequences."
One good piece of news: There are a large number of new treatments for macular edema and retinopathy. The most recent FDA approval came this year for Iluvien, an implant that delivers corticosteroids to the eye for three years to reduce swelling. Earlier corticosteroids had to be injected into the eye every three months. There is also a series of antivascular endothelial growth-factor drugs (anti-VEGF), which prevent a group of proteins in the retina from promoting the growth of abnormal blood vessels, including Ranibizumab (Lucentis), Bevacizumab (Avastin), Afilbercept (Eylea), and Ozurdex (Dexamethasone).
"There's a lot of research in the pipeline for new treatments. We're looking at a lot of different pathways to suppress the disease," said Ho. "Still, it's very important to make sure that the patients control risk factors as best as possible. Making good decisions about what you eat, walking 30 minutes most days of the week, controlling blood pressure, monitoring blood sugars, and making sure the A1C - a three-month average of blood-glucose readings - is in the 6-to-7 range is vital."
Since her complications, Turner has taken better care of herself, going on an insulin pump, exercising regularly, and watching her diet.
"I don't want my story to be a scare tactic," said Turner. "Growing up with diabetes, it's far too common to point to the potential of these horrible things happening. But thinking about complications is paralyzing to me.
"If anything, what I've learned is if I do deal with my diabetes, I feel better and stronger about myself. Focusing on the benefits of being vigilant about your diabetes care is more beneficial than thinking about the potential complications."
215-470-2998