LEHB works to keep police health-care costs under control
Amber DiMarino, Joe Hinchliffe, and Phyllis Squillaciotti thought something was off. Reviewing medical bills for Philadelphia police, the trio repeatedly noticed two bills for visits to the eye doctor on the same day.
Amber DiMarino, Joe Hinchliffe, and Phyllis Squillaciotti thought something was off. Reviewing medical bills for Philadelphia police, the trio repeatedly noticed two bills for visits to the eye doctor on the same day.
So about three years ago, they ran a report for the 23,000 police employees and their families covered by the department's health-care plan. Ka-ching! The three found $94,000 in double billing over two years for vision claims, some of which turned out to be fraudulent.
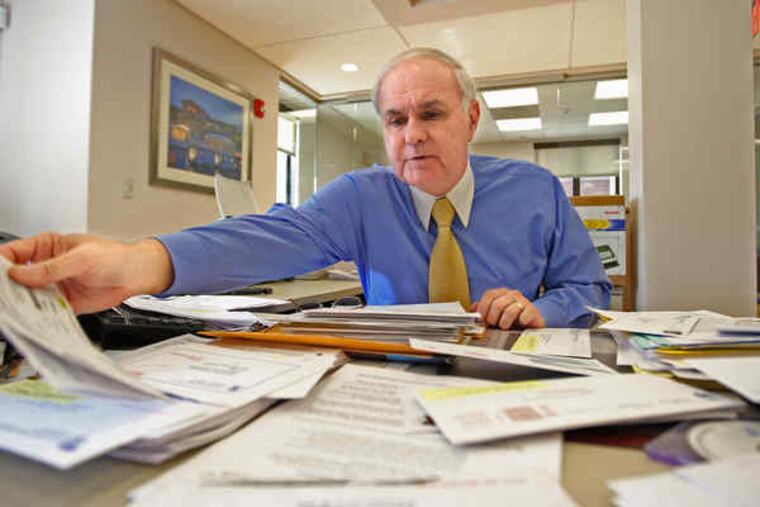
DiMarino, Hinchliffe, and Squillaciotti are not detectives, at least not in the usual sense. They belong to a team of claims reviewers at Law Enforcement Health Benefits Inc., which oversees health-care benefits for Philadelphia police. LEHB and its administrator, Thomas Lamb, are roundly praised for aggressively reining in costs.
The arbitration panel that awarded the most recent contract between the police and the city in December called LEHB "one of the most effective and efficient health-care programs in the commonwealth."
Mayor Nutter, who has struggled to make health-care cost reduction a pillar of his administration, said, "Tom is excellent at what he does. Everyone knows that."
Even so, LEHB's efforts cannot offset city health-care costs that are high relative to other employers', mostly because Philadelphia employees pay little out of their own pockets. That leaves taxpayers shouldering health-care costs that jumped 123 percent from 2001 to 2008, a period in which city revenue rose only 38 percent.
Union leaders say they have negotiated better benefits in lieu of wage hikes over the years, and some research shows that, packaged together, Philadelphia's wages and benefits are in line with those in other cities.
Starting in July, Lamb will be at the forefront of a new effort to control medical costs known as self-insurance. Instead of paying a premium to its insurer, Independence Blue Cross, LEHB, using city funds, will now pay claims as they come in. The city hopes to save about $5 million in fiscal 2011 because of the switch to self-insurance.
When Lamb, 64, left his job as a traffic cop in 1989, health care wasn't the mess it is today. But as expenses escalated in the 1990s, he decided that if he didn't take on costs, his members could start losing benefits.
"It would be much easier to sit here and not do anything and say, 'Just raise the co-pay,' " Lamb said. "It's not Blue Cross' money. It's the union's money, so it's our responsibility."
He has two weapons: intense communication with his members, and mining health-care claims for mistakes and fraud.
His team calls every member at least twice a year to see how he or she is doing.
Those checks helped Bill Wynn avoid surgery for what was initially diagnosed as a brain tumor after part of his face started drooping in 2005. When Wynn called LEHB, the fund urged him to work with Guardian Nurses, a Flourtown company that has a contract with the police fund and does advocacy work for patients.
Wynn's doctor had told him surgery could make sense to remove the tumor while it was small, but Guardian sent him to another expert who said he could wait to see how quickly the tumor grew. A year later, a new MRI showed that the spot that originally led to the tumor diagnosis had disappeared - no tumor, no surgery.
"I would certainly agree that the LEHB did a great service to me, and it saved me from making a wrong decision," Wynn said. "And can you imagine what that surgery would have cost?"
Now retired from the police force, Wynn traded in unused sick time to keep his insurance with LEHB.
LEHB also offers seminars on such topics as how to discipline children and sends out fliers about others, such as managing asthma and controlling diabetes. The messages are about as subtle as red-and-blue flashing lights: "Your Children Will Miss You!" reads one flier about the risks of obesity that encourages members to join an LEHB walking club.
Lamb focuses many efforts on smokers and people with diabetes because they contribute heavily to the fund's costs. He has backed away from ideas that seemed too aggressive, such as asking smokers to push around an oxygen tank for a while.
He uses positive incentives, too. People who joined the walking club got $25 each.
His administrative budget for 10 full-time and two part-time employees, according to the fund's 2007 filing with the U.S. Labor Department, is $1.4 million. His earnings were $136,584, which includes reimbursement for vacation and other days that he doesn't take.
The city's union structure means its employees are covered by five different health-insurance plans, each separately run, making it difficult for Philadelphia to implement Lamb's strategies throughout the workforce.
In addition to regular communications with members, Lamb's program includes 49 reports generated monthly that look for everything from possible fraud to double billing. The "Coordination of Benefits" report looks for claims paid by LEHB that should have been paid with different insurance. Maybe a member has retired and is now insured by Medicare, for example.
The "Baby Report" tracks newborns to make sure LEHB doesn't pay twice for the same service when a child originally called "Baby Boy Doe" becomes "John Doe."
Lamb and his team calculate a "hit rate" for each report, based on the dollar value of questioned claims and dollars returned to LEHB. In the last two years, for example, the "Coordination of Benefits" report has generated $7.5 million in contested claims, $5.5 million of which has been returned to LEHB. The remainder is under review.
"If it's measurable, we measure the return on investment," Lamb said.
The vision investigation resulted in a 2008 guilty plea by Bucks County optometrist Samuel Young for about $4,800 in fraudulent claims, and Independence Blue Cross has turned over two other vision-claims cases to prosecutors.
"I wish I had 100 Tom Lambs," said Larry Kissner, vice president of sales and marketing for Independence Blue Cross. "On literally every claim, he really digs into the data."
Lamb has a number for that, too: 250,000 claims, on average, reviewed monthly. The number is so high because it includes each service at every visit, multiplied by the number of times it turns up in one of LEHB's 49 reports.