Penn researchers are studying how to prevent breast cancer recurrence, which is often fatal. Their work just got a $10 million grant.
In a phase II clinical trial, 80% of participants treated for dormant cancer cells remained cancer-free four years later.
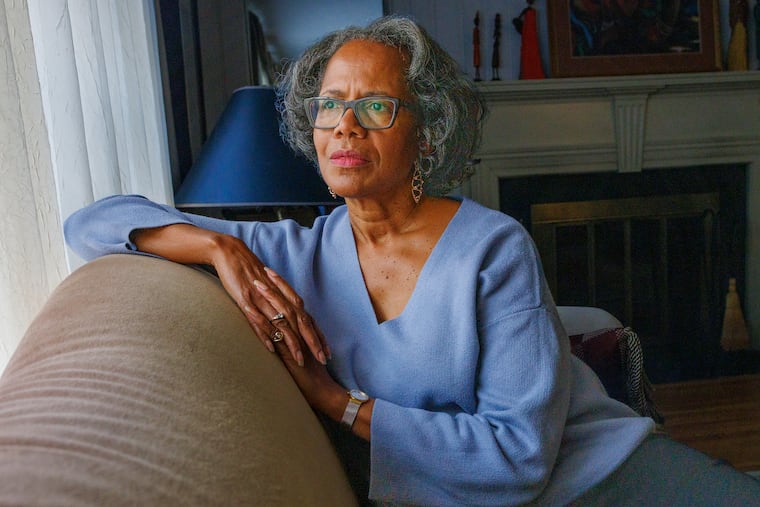
Just as she hoped to start a family, Denise Murray was diagnosed with an aggressive form of breast cancer. Thirty years old and newly married, she felt it was too risky to consider pregnancy if she might not live to raise her children.
A majority of patients, including Murray, whose tumors are found early, are still alive five years later. But in about 30% of cases, breast cancer eventually returns — sometimes years or even decades later — and then is almost always fatal.
Doctors have no way to definitely say whether or when a patient’s cancer may recur. But researchers at University of Pennsylvania now think they are learning how to find and kill dormant breast cancer cells left in the body after treatment, before they have a chance to reactivate and spread. After four years, all but two of 51 patients treated in an advanced clinical trial are still cancer-free.
The early findings, presented at a European oncology conference in October, offer hope that treatment may one day reduce the likelihood of breast cancer fatally recurring. Now, with a $10 million federal grant to expand their proof-of-concept trial, Penn researchers seek to give patients greater certainty that they do not have to live in fear of their cancer returning.
“When you make these decisions, you don’t make them for yourself, you make them for your family,” said Murray, who lives in Egg Harbor Township. “They have to pick up the pieces of whatever happens.”
Angela DeMichele, the co-director of the breast cancer research program at Penn’s Abramson Cancer Center, began researching breast cancer recurrence after struggling with how to talk to patients about the unknowns that remained after treatment.
“We get to the end of the initial treatment and they say, ‘How will I know if it worked? What do you mean I have to just wait and see?’” she said. “They’re just waiting for the other shoe to drop their whole lives.”
Finding and killing dormant cancer cells
After treatment, it’s common for some breast cancer cells to go dormant — to exist in the body without multiplying and creating masses the way cancer cells normally do. For reasons doctors still haven’t figured out, these dormant cancer cells sometimes “wake up” and begin to rapidly divide again months, years, or even decades after treatment.
DeMichele compares the phenomenon to bear hibernation: Bears go months without eating or drinking, their heart rate slows, and they remain sedentary through the long winter. Then one day, they wake up famished and emerge from their den to prowl the forest for food.
Doctors have for years known that these dormant cancer cells settle in bone marrow, the spongy center of bones where red blood cells are made. Recurrent breast cancer is almost impossible to eliminate because once it has reached bone marrow and blood, it spreads everywhere.
DeMichele and her colleagues set out to answer two questions: First, could they detect dormant cancer cells by periodically testing patients’ bone marrow? Second, could a combination of oral medications that don’t work against active cancer kill the cells while they were dormant?
Putting life on hold for cancer
Murray knew immediately that she wanted to enroll in the trial because it was at least a chance at the type of certainty she needed to plan her future.
At age 13, Murray had been treated with chemotherapy for lymphoma, a blood cancer thought to be unrelated to her breast cancer diagnosis. The chemotherapy she received in childhood had made it more likely that she would experience infertility. Now, additional chemotherapy and radiation could damage her reproductive health.
Before beginning her breast cancer treatment, Murray and her husband decided to freeze embryos. The procedure entails removing eggs from an ovary, fertilizing them in a lab, allowing them to grow several days into embryos, then freezing them for future use.
She had a lumpectomy, chemotherapy, and radiation, then enrolled in the trial to test her bone marrow for signs of dormant cancer cells.
As part of the clinical trial, doctors extracted samples from patients’ pelvic bone — a reservoir rich with bone marrow — and tested them for dormant cancer cells.
If the test came back positive, patients were given oral medications.
Roughly 200 people enrolled to have their bone marrow tested, and 51 were ultimately treated for dormant cancer cells. About half of the 51 had triple-negative breast cancer, which has a higher rate of recurrence than less aggressive forms. All but two remained cancer-free four years later.
Next steps in detecting cancer before it recurs
With a $10 million grant from the Department of Defense, DeMichele and her colleagues will enroll more patients, especially from diverse backgrounds, and continue testing past participants.
One of the trial’s first patients, Lisa Dutton, 63, of Wynnewood, is now helping to encourage more people to participate in studies like this one. Dutton enrolled after she was diagnosed with breast cancer in 2017. A bone marrow test found dormant cells in 2021, so she started the trial’s drug regimen. She’s still cancer-free today.
She’s grateful a friend encouraged her to join the trial. Dutton, who is Black, now volunteers with an advocacy organization focused on outreach aimed at improving racial diversity in clinical trials. Dutton fields phone calls from people who want to know what it’s like to participate, or who need reassurance that they’ll still be treated for their cancer, even if they don’t receive the supplemental therapy being tested.
Dutton said she hopes that by sharing her experience with others, she can be “an example for people to see there could be a light at the end of the tunnel,” and that clinical trials are worth considering, even if they may lead to additional treatment.
Enrolling more patients from diverse backgrounds is critical for DeMichele’s team to advance their work.
The initial study provided proof-of-concept, but her team needs to test the theory with many more patients before they can know if they’ve found a way to detect and intercept dormant cancer cells.
“We would like to have a strategy to be able to say, ‘You are free and clear,’” DeMichele said. “Wouldn’t it be amazing?”
‘Pure joy’
Murray tested positive for dormant cancer cells a few months into the trial. She was disappointed, but also relieved that doctors could offer a way to kill off the cells — hopefully for good.
Her next bone marrow test after completing the drug regimen came back clean. And so did the next.
She’d carried the weight of cancer for so long, but now feels she has better information to guide her future.
In October 2019, Murray gave birth to her daughter, Savannah, who became a big sister two years later.
“Joy,” Murray recalled feeling while holding her baby girl for the first time. “Just pure joy.”