CDC: Opioid guideline not meant to limit cancer patients’ access to painkillers
Opioids are a mainstay of pain relief for cancer and sickle cell patients. The CDC's prescribing guideline has been improperly used to limit their access.
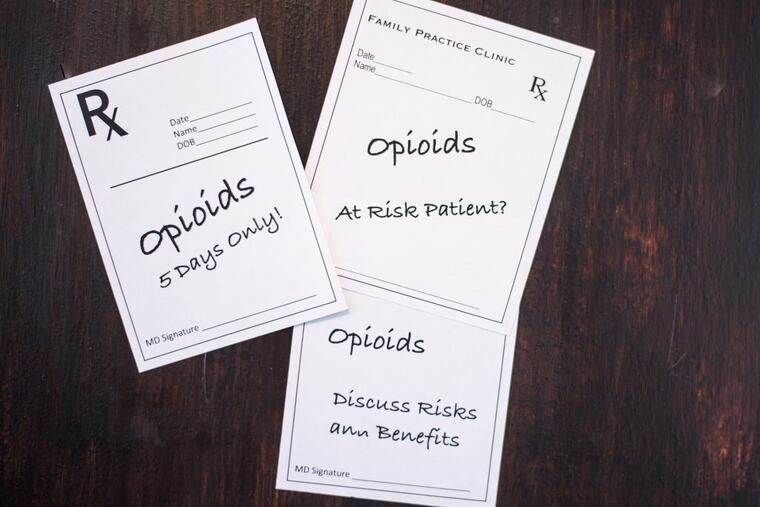
Some measures intended to curb the nation’s opioid addiction epidemic are making it tough for patients with cancer and sickle cell disease to get access to painkillers.
This week, three oncology organizations announced a development they hope will improve the situation: The U.S. Centers for Disease Control and Prevention said its 2015 opioid prescribing guideline was never intended to deny the therapy to patients suffering acute or chronic pain caused by cancer or sickle-cell disease, a severe hereditary form of anemia.
The clarification came in a February letter from Deborah Dowell, a top CDC medical officer and lead author of the guideline, to executives of the National Comprehensive Cancer Network, the American Society of Clinical Oncology, and the American Society of Hematology. They all met late last year to discuss the problem of conflicting recommendations for prescribing long-term opioid therapy to cancer patients.
“This clarification from the CDC is critically important because, while the agency’s guideline clearly states that it is not intended to apply to patients during active cancer and sickle-cell disease treatment, many payers have been inappropriately using it to make opioid coverage determinations for those exact populations,” said ASCO chief executive officer Clifford Hudis.
To gauge the impact, the American Cancer Society’s advocacy arm sponsored national surveys of cancer patients and survivors. Between 2016 and 2018, the fraction of patients who could not get insurance coverage of an opioid prescription rose from 11 percent to 30 percent. In addition, many more patients reported restrictions on the number of opioid pills and refills, and problems finding a pharmacy to fill the prescriptions.
NCCN chief executive officer Robert W. Carlson said the CDC clarification letter will be posted on the websites of oncology and other medical organizations so it can be used by physicians and patients who are fighting opioid prescription denials.
Carlson noted that NCCN has published prescribing guidelines that help cancer specialists assess the risk of opioid abuse “while still ensuring people with cancer don’t suffer unnecessary, severe pain.”