Systemic racism is a public health issue. Community health workers are proven to help.
Treating race inequities like a public health problem requires specific actions, and mobilizing community health workers is one example.
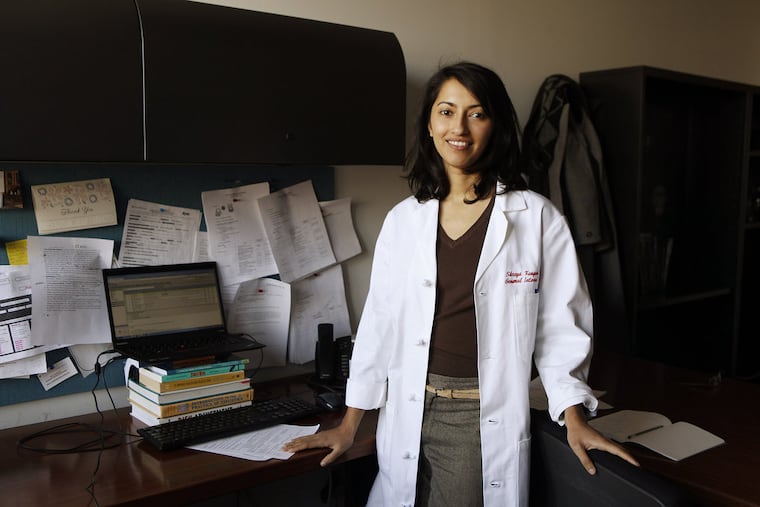
Ask Cheryl Garfield how racism damages the health of Philadelphians, and she tells the story of a Black man who recently turned up at a city hospital. Unemployed, uninsured, and homeless, he relied on a walker because he has gout, in addition to heart failure and high blood pressure.
The man, one of Garfield’s clients at the Penn Center for Community Health Workers, was on Social Security, but his benefits were cut off because he had no way to get to the local office for evaluation of his disability.
People of any race could face his predicament, but such situations are far more prevalent among people of color, experts say, for a host of reasons that can be best described as systemic racism, a public health pandemic that existed long before the coronavirus pandemic.
Put simply, systematic racism influences health because of how for decades it has led to unequal access to opportunities for even the most basic needs, such as quality education, nutritious and affordable food choices, a living wage, and clean air and water.
“Basically, when it comes to racism, certain things get done for certain people,” said Garfield. “At all levels across the city, you have patients across the city who will be turned down from services because they are African American.”
What Garfield sees in Philadelphia is well-known to national experts.
“We have long known racism as a key driver of health,” said Regina Davis Moss, associate executive director of public health policy and practice for the American Public Health Association. “To achieve health equity, you have to address racism as a public health crisis.”
But the pandemic is revealing this crisis so starkly, with COVID-19 cases striking minorities disproportionately around the nation, public health experts hope the problem will at last be addressed, and not explained away as the result of poverty or poor choices. Locally, the smallest difference has been observed in Philadelphia, which has seen 45 cases per 10,000 Black residents, compared with 31 cases per 10,000 white residents. In other counties, the difference is larger. For instance, Delaware County has experienced 131 cases per 10,000 Black residents compared with 58 cases per 10,000 white residents.
“In the broadest sense, no matter what the disease — coronavirus, hunger, or chronic diseases — the same people are always at risk: people who have been systematically oppressed because of their race or other aspects of their identity,” said Shreya Kangovi, associate professor of medicine at the University of Pennsylvania Perelman School of Medicine and founding executive director of the Penn Center for Community Health Workers.
Getting to the root
Treating race inequities as a public health problem — much in the way that gun violence is being approached as a health issue — implies that the disparities racism creates can be prevented through specific actions.
» READ MORE: Philadelphia has a gun violence epidemic. What if it were treated like any other contagious disease?
“As we define the problem statement, the thing we need to solve is injustice,” Kangovi said. “We can’t always just have disease-specific interventions – those are treating the symptoms. We have to get close to the root.”
That root starts when marginalized communities are not listened to, employed, or empowered in some way, Kangovi said. Collective actions — or failures to act — influence living conditions, which subsequently influence behaviors and health. Treating these inequities involves correcting the fundamental ways that communities are treated differently.
Addressing centuries of unequal treatment requires intervention at all levels of society, even as seemingly small as reporting statistics by race, experts say. At the public health level, one approach that is finding success, by literally meeting people where they are, involves community health workers.
Community health workers are trusted, respected people who have had some of the same experiences in life as the people they serve. So their recommendations often are better accepted than if they had come from physicians and nurses who may not understand, for instance, the specific challenges of getting more exercise when you live in a neighborhood where it’s dangerous to walk.
They provide a wide array of services for people including health coaching, social support, and navigation, and get to know the stories of their clients and address their medical and life issues.
“What compels me about community health workers is they are very close to a solution at the root of the problem,” Kangovi said. “They are often members of groups who have been systematically oppressed, and despite the adversity and what they’ve been through, they advocate for other people.”
Advocacy for clients takes many forms, whether it’s getting them into good primary care, applying for Medicaid or Social Security, or holding their place in line at a community health center so they can be one of the first ones seen. And these actions are a step to ensure people can receive the same services as those with greater resources.
» FAQ: Your coronavirus questions, answered.
Above and beyond
Community health workers like Garfield strive to correct these disparities. Garfield said most of her patients are Black people who live in South and Southwest Philadelphia. They have no access to big supermarkets and rely on corner stores, so they usually can’t get fresh, healthy food. Many have to decide whether to pay for their rent, medications or their food, a no-win choice that can mean getting so sick they end up in the emergency room. For people in her care like the homeless man with chest pains, Garfield goes well beyond the usual health-care job functions. In his case, she put in the application for him to get pandemic emergency funds — and a mailbox where it could be sent.
Community health workers have also been paired with police officers to teach them how to be antiracist and respond holistically to the issues they see. The same approach can extend to training other health-care professionals. Indeed, Philadelphia has seen numerous public and private demonstrations of how doctors and nurses are pushing to address race-based inequities at all levels of their profession. The area’s hospitals recently signed a letter, affirming that racism is a health-care issue and committing to improving access to care for underserved communities among other actions.
» READ MORE: Thousands of medical workers turn out to remember George Floyd and work for health equity
Even from a business perspective, community health workers pay off, with studies showing that their work helps clients avoid unnecessary hospitalizations and reduce emergency-room visits, saving taxpayers significant amounts on Medicaid.
Despite all the evidence and knowledge about how to deploy them, there are only 58,950 community health workers in the United States — about one for every 5,500 Americans. Experts stress that more are needed to address health disparities. Hiring more community health workers could also support local COVID-19 recovery efforts.
“The missing piece is financing,” Kangovi said. “Most community health workers are paid through mechanisms like grant funding.”
Advocates are calling on Congress and the Centers for Medicare and Medicaid Services to act on this need. Altogether, responding to health inequities requires putting more resources where they are needed, and public health and a workforce of community health workers is one example.
“If you look at funding for law enforcement vs. public health — you will see a vast difference that reflects how we value these systems,” Davis Moss said. “We’ve got to address the social determinants of health, of which racism is just one. We have to act best at all levels if we want that change.”