How a Pennsylvania doctor stopped a virus outbreak in 1934 — with blood
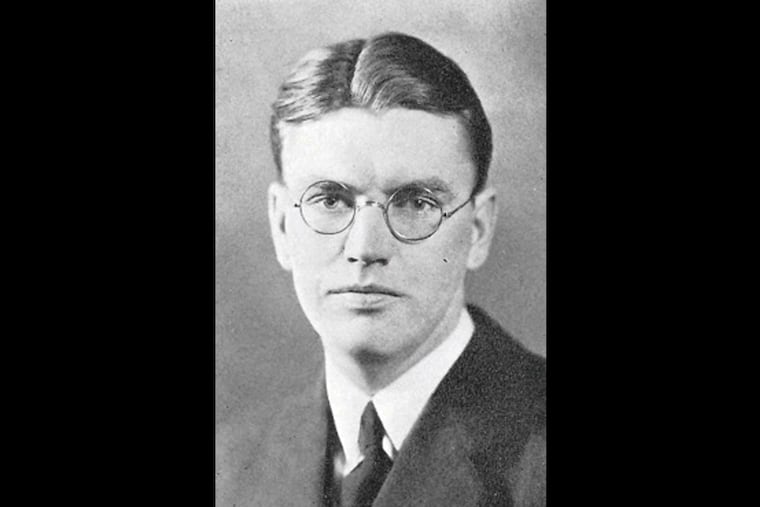
J. Roswell Gallagher administered “serum” to students at the Hill School in Pottstown. In China, the same technique was recently used against the coronavirus.
In January 1934, officials at the Hill School learned that a student had been exposed to measles over winter break and confined him to the infirmary.
This was no idle precaution by J. Roswell Gallagher, the staff physician at the private boarding school in Pottstown, Montgomery County. Back then, the highly contagious disease killed hundreds of people each year in the United States. (A vaccine would not be developed for decades.)
Yet it was not enough. The student, identified only as C.Y. in a medical journal at the time, developed symptoms and infected two schoolmates who were being treated for other illnesses in the infirmary. And before those two developed symptoms, they were discharged to their dorm rooms, exposing dozens more students.
Gallagher then took a decisive step that has relevance for how the world responds to another infectious disease in 2020: the new coronavirus. He extracted serum from the blood of the initial patient — reasoning that it contained antibodies produced by the boy’s immune system — then infused it into the bodies of 28 other students who had not previously had the measles.
None of them got sick.
Gallagher was not the first to try this approach against viruses, but his effort was unusually successful, providing important clues about the proper dosage and timing of such infusions, said Arturo Casadevall, chairman of microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health.
“It makes perfect sense,” Casadevall said of the underlying concept. “But this is really forgotten history."
Serum also was used to prevent and treat bacterial infections, in some cases extracted from the blood of animals, but the practice largely fell out of favor by the mid-20th century with the advent of vaccines and antibiotics.
This year, Chinese physicians have revived the concept to help fight the coronavirus, with promising early results, Reuters reported. Instead of using serum to treat the infection, physicians used blood plasma that had been extracted from recovered patients. (Serum and plasma both consist of fluid that remains after blood cells have been removed, but they are prepared differently.)
Mike Ryan, the head of the health emergencies program for the World Health Organization, called the approach “a very important area to pursue.”
Casadevall, who described the Hill School episode in a recent commentary piece for the Wall Street Journal, said he had heard preliminary discussions among U.S. infectious disease specialists about whether to try the approach against the coronavirus here.
A key determinant will be how well the coronavirus can be staved off with other measures, such as antiviral drugs and isolation of patients, he said. Even better would be a vaccine, but none is ready for use.
Administering antibody-laden plasma or serum to nurses, physicians, and ambulance workers would be a reasonable idea, the Hopkins scientist said. The treatment would not confer the lasting protection of a vaccine but would enable recipients to fight off an infection for several weeks, he said. Other likely candidates for such a treatment would be family members of infected people.
“You could sort of create a ring of immunity,” he said.
In 1934, Gallagher was operating at a distinct disadvantage to physicians of the 21st century. He had no way to measure the levels of antibodies in the blood of the three infected students at the Hill School. Nor did he have modern equipment to screen their serum for viruses.
Drawing from the experience of others who had tried serum therapy, Gallagher extracted blood from the initial patient on the 10th day after his temperature had returned to normal, reasoning that the boy’s serum would still have a high level of antibodies from fighting off the disease — yet no virus.
But the doctor needed more serum than what he was able to obtain from the initial patient, he reported in the American Journal of Public Health. He identified a total of 66 students who needed serum because they met two criteria: They had never had measles and had contact with students who did.
So he ordered additional serum from a New York laboratory. The lab serum was administered to 37 students, while 28 were treated with serum extracted from the initial patient. One student was not treated, for undisclosed reasons.
The 28 students with the patient’s serum all emerged unscathed. Three of the 37 students who got the New York serum suffered mild cases of the disease.
Gallagher speculated that lab serum contained a lower level of antibodies than the serum from the patient, likely because the latter was only 24 hours old.
Without advanced laboratory equipment, he would never know. But with the tools he had available, Gallagher earned a place in public health history.
Gallagher went on to a long career at what is now called Boston Children’s Hospital and later Yale University. He is credited with pioneering the field of adolescent medicine, arguing that teens should be treated differently from children and adults.