A Philly ER doc’s take on why fat is not the enemy and how cardiologists are like plumbers
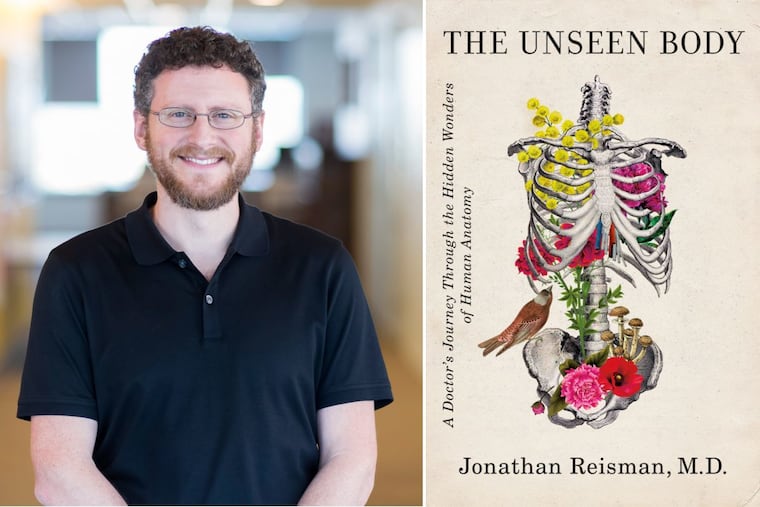
Jonathan Reisman draws on his voracious curiosity and background as a naturalist to explore the amazing workings of the human body.
When Jonathan Reisman treats patients in the emergency room, a lot is going on in his head beyond what he learned in medical school.
The physician, who lives in West Philadelphia, studied math in college. He then spent five years in Russia, studying forestry, water quality, and anthropology, and working as a translator for outdoor adventure tour groups. He has developed a keen interest in outdoor survival skills, teaching himself which mushrooms are safe to eat and how to tan animal hides. He has gone to sea on an Indigenous whaling boat.
All of it comes into play in The Unseen Body (Flatiron Books, $27.99) in which he takes readers on an organ-by-organ journey through human anatomy, drawing parallels with natural phenomena and his world travels.
A graduate of Rutgers Robert Wood Johnson Medical School, Reisman, 40, works as a pediatric emergency medicine physician at Cooper University Hospital in Camden, and also does emergency room shifts at Schuylkill Medical Center in Pottsville and at Lehigh Valley Hospital-Pocono in East Stroudsburg.
We interviewed him about what he admits are his “offbeat perspectives” on the field of medicine.
In one hospital where you worked, you asked the head of maintenance to give you a tour of the building’s plumbing system. What did you learn?
I learned that when there’s a problem with the plumbing, that the plumber solves the problem in the same way a cardiologist solves the problem of a heart attack. When the water pressure drops in the whole hospital, it tells him something different than if it just drops in one particular wing or one floor of the hospital. It’s that regional vs. global problem. Zeroing in on where the blockage might be, where the problem is, involves understanding the branching of the pipes that feed the whole hospital, or the arteries that feed the heart.
Was he surprised when you approached him?
He was. I was, like, “Hey, I’m writing this book. Can you show me where you work and how you solve problems?” I was the first doctor to go into this room he called the valve room. It was the heart of the hospital’s plumbing. He spent an hour giving me a tour. He probably still thinks I’m a little strange. He showed me what I would call the arteries — the supply of fresh water to the hospital, and what I would call the veins — draining wastewater under gravity.
As a lifelong naturalist, you described the kidney in terms of its role in the body’s ecosystem. What prompted that idea?
I call it a keystone species in the book. That’s an ecological term for a species on which an entire ecosystem can rest. When that keystone species is reduced in number, it can bring the whole house of cards crashing down. Kidneys are the first to get injured in severe illness. They’re one of the first things that start to fail. I compare it to a canary in the coal mine. Often, kidney failure is what we look for first in people with severe overwhelming infection, or what we call a cytokine storm.
From an ecology perspective, the kidney also purifies, much like wetlands act as a buffer against changes in water level and pollution, sucking up toxins and helping to protect inland waterways from salt.
Years ago, you went to sea on an Iñupiat whaling boat. Describe how you gained new appreciation for the beneficial side of fat.
When I finished medical school, fat was always portrayed as the enemy. That goes for fat in our diet, fat in the bloodstream in the form of cholesterol and triglycerides, and fat on our bodies in the sense of obesity. When I was in Alaska and learned about the traditional culture and diet, I found that fat was a humongous part of their lives. More than half of all calories is animal fat. No greens or vegetables. And if you go far enough north, there are no berries.
For them, fat was the single thing that allowed human beings to even live in such a harsh environment. Fat is like the currency in the Arctic. Yet they actually have very low rates of cholesterol and heart disease. Now that they’ve partly switched to a modern American diet, they suffer from the same diseases as all the rest of us. I think the science of nutrition is only beginning to understand fat and its role in health and disease.
You wrote that one part of the human body seems especially vulnerable and badly designed: the throat. How would you fix it?
It would be much better if the windpipe for air, and the esophagus for food and drink and everything else — it would be more convenient if they were not right next to each other.
Every time we swallow, unconsciously, all day, every day, if you swallow incorrectly just one time, you could die [from choking or aspiration pneumonia]. It seems like a really stupid design. The muscles and cranial nerves are part of this very orchestrated system. It’s very coordinated and perfectly timed so that the tongue moves upward just as the food is passing over the windpipe. … That plugs it so that food can flow right past it without going in.
When you learn some of these of things in medical school, you sort of become amazed that it works as well as it does. In a similar way, when you find how sperm and egg find each other, it is miraculous that it ever works at all.
Given your background in mathematics, do you find that both your fellow providers and patients could use a refresher course in statistics?
So could I, honestly. We’ve all gotten a crash course in statistics over the last two years [with the COVID-19 pandemic].
For me and a lot of my classmates, statistics was the hardest class in medical school. It doesn’t come naturally for people to think that way. It takes a lot of training. The trip that took me to Alaska, I was there studying infectious disease in native people. Epidemiologists, when they design studies, the biggest thing they do is trying to figure out how to control for variables that might affect their results. You have to pull this stuff out of the real world and create an artificial environment to get a result. I don’t blame anyone, either medical professionals or patients, for struggling to understand a lot of the public health concepts.