Inspira soars — and scrambles | Philly Health Insider
And more deets on West Nile virus in Philly
This week, we go inside Inspira Health, exploring how one South Jersey health system can serve some of the state’s most lucrative and poorest communities. Plus, we tell you what you need to know about the future of noncompete agreements for clinicians, three Philadelphians developed West Nile virus (and its rare neurological side effect), and we break down the region’s busiest emergency departments. (See how yours compares.)
But before we dive in: an introduction. I’m Alison McCook, and I am the newest member of the Inquirer’s health team, but no stranger to writing about medicine and science. I’ve been a health reporter for 20 years, writing for Science, Nature, and other industry publications. I was the deputy editor at life sciences mag The Scientist (then based at 400 Market St. in Philly), and the editor of Retraction Watch, which investigates academic publishing and misconduct.
I’m thrilled to bring my experience to my hometown paper (born in Chestnut Hill, raised in Springfield Township in Montgomery County). I’ll be working with Aubrey on the weekly newsletter, plus covering academic research, biotech, and related topics. If you have any thoughts or tips, email me here.
📮Is the legal seesaw over non-compete agreements stressing you out? For a chance to be featured in this newsletter, email us back.
If someone forwarded you this newsletter, sign up here.
— Alison McCook, Inquirer health reporter, @alisonmccook.
The nonprofit health system’s experience in South Jersey in recent years has been wildly different across its four general hospitals.
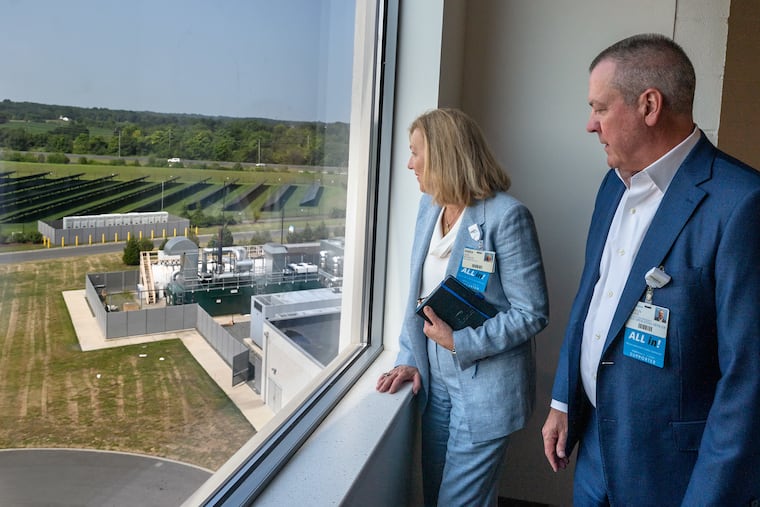
At its Gloucester County facility, for instance, high patient demand has forced the company to embark on a $220 million expansion. “We never had any concept that we’d see this much growth this fast,” Amy Mansue, Inspira’s CEO, told our colleague Harold Brubaker.
But in neighboring Salem County, its two small community hospitals are less than half full.
What gives?
The answer, not surprisingly, is demographics: Gloucester County has experienced significant population growth in recent years, bringing residents with private insurance that can pay for more care, while Salem and Cumberland Counties, home to other Inspira providers, struggle with poverty, too few doctors, and poor health outcomes.
But unlike other large nonprofit health systems, Inspira has no plans to pull out of poor communities. Read more to find out how Inspira got where it is today (including its new 80,000-square-foot outpatient center in a former Dick’s Sporting Goods in Deptford), and its plans for the future.
The latest news to pay attention to
Don’t rip up your employment contracts just yet — last week, a federal judge in Texas struck down an April ruling banning noncompete agreements, set to kick in next month. Noncompete agreements, which affect many health care workers (including nearly half of all doctors), prohibit clinicians from working for competitors. So in the crowded Philly health-care market, changing jobs could mean changing cities. We have the scoop on what this means for you.
Three Philadelphians have been diagnosed with West Nile virus. All developed a serious neurological condition, a rare side effect of the mosquito-borne virus that occurs in less than 1% of patients.
Thomas Jefferson University’s Medicaid insurance arm scored a win last week, in the form of a contract to manage long-term care benefits for some of the 380,000 Pennsylvanians who participate in the $5 billion program called Community HealthChoices. The program covers long-term services (such as nursing homes and home care) for low-income seniors and disabled people who qualify for both Medicare and Medicaid.
This week’s number: 660,000.
That’s the minimum number of annual patient visits reported by Philly’s 11 busiest emergency departments, collectively.
Some of the busiest hubs for emergency care include Cooper University Hospital in Camden, Temple University Hospital in North Philadelphia, the Hospital of the University of Philadelphia in West Philly, and multiple Jefferson Health hospitals on both sides of the Delaware River. Each receives more than 60,000 patients a year.
In contrast, three other facilities — Crozer Health’s Delaware County Memorial Hospital (no longer offering emergency services), Prime Healthcare’s Suburban Community Hospital, and Lower Bucks Hospital — all get fewer than 19,999 ED visitors per year. (All are financially struggling; the Prime hospitals have begun renting unused hospital space as movie sets.)
Read on to see how busy your local ED is.
Each week, we highlight state inspections at hospitals in our region. Up this week: Paoli Hospital. Inspectors visited the Chester County hospital (part of Main Line Health) twice to investigate potential safety problems between December 2023 and May.
In one February incident, state inspectors found Paoli Hospital had mismanaged anesthesia in a patient’s case, but did not cite the hospital because the problems were fixed before inspectors arrived.
Click here to read more about the details we could gather about the incident.
📮Are you privy to additional information about the incident at Paoli Hospital or other inspection issues at Philly-area hospitals? We’d love to learn more, email us back.
What are the biggest concerns of Philadelphia-based physicians?
In a recent interview, Abraham Gutman spoke with John Vasudevan, outgoing president of the Philadelphia County Medical Society.
During his tenure at the organization — which represents all physicians in our area, regardless of affiliation or career stage — Vasudevan received an earful about the pain that local docs feel when their medical decisions are undermined by insurers. “Physicians love their job when they feel that their ability to have an autonomous decision about how to care for patients,” he told Abraham.
Read more about the sports medicine physician at Penn Medicine’s experience heading the society.
Jefferson’s top emergency medicine doctor is stepping down from his longtime chair position.
A Jefferson spokesperson told reporter Wendy Ruderman that Theodore Christopher’s move is “a planned semi-retirement.” He will continue to serve as a faculty member at the Sidney Kimmel Medical College and a practicing physician on Jefferson’s medical staff.
Christopher was investigated several months ago for failing to follow hospital policy by leaving work without calling for backup to cover his shift; he was supposed to be supervising a first-year resident who was only four months into her training as an emergency medicine doctor. According to Jefferson, Christopher left work that day due to an emergency gastrointestinal issue, and no patients suffered harm.
As a founding member of a national research partnership focused on cancer immunotherapy, UPenn will get a piece of a new $125 million award.
The Parker Institute for Cancer Immunotherapy announced last month that it would invest the money in research efforts, clinical trials, and training for early-career scientists at Penn and other members of the organization’s network. The money will be distributed as grants over the next five years.
By submitting your written, visual, and/or audio contributions, you agree to The Inquirer’s Terms of Use, including the grant of rights in Section 10.